
Restoring ICU stability through Lean
CASE STUDY – How lean concepts and practices are addressing and reversing increases in hospital infections, staff absences and transfers in the intensive care units of this Brazilian hospital.
Words: Samir Khatib, Physician and Coordinator of the Intensive Care Units (ICU), Hospital de Amor
Planning, structuring, and executing efficient work management is increasingly crucial in the Intensive Care Units (ICUs) of large hospitals. This directly affects patient safety, quality of care, team well-being, and operational costs.
In this context, the Hospital de Amor (HA), better known as the Barretos Cancer Hospital, located in the interior of São Paulo state, recently embrace Lean Thinking and Practice to promote significant improvements in work management within its ICUs. The lean initiative was carried out to reverse problems caused by a recent restructuring of work teams.
The hospital currently has two ICUs—each with 10 beds and a team of five technicians and up to two nurses. Recently, with the objective of reducing costs, work schedules in this sector were modified to eight-hour shifts. Previously, shifts ranged from 6 to 12 hours. Breaks were also changed: they used to be 15 minutes long and they now last one hour.
This new reality placed the ICU in a new operating condition in which, during each 8-hour shift, the care structure was at times insufficient to meet demand, with a labor deficit of up to 62% compared to the ideal capacity, compromising the continuity and effectiveness of the care provided.
This generated a series of challenges: increased operational costs, reduced quality of care, a higher incidence of adverse events, increases in healthcare-associated infections (HAIs), as well as widespread team dissatisfaction, including an increase in work absences through medical leave due to health problems among professionals.
The lean implementation aimed to understand these problems, investigate their root causes, and propose countermeasures, with the aim to improve the stability of care processes and team satisfaction, reducing HAI notifications by 30% and work absences due to medical leave by 50%.

INVESTIGATING THE SITUATION
The analysis of the current state revealed a multifaceted scenario in which the adjustment of working hours directly impacted operational results. In 2024, the hospital’s ICUs had an occupancy rate close to 90%. Patient classification by severity category was divided into low (25.23%), intermediate (25.43%), high (20.79%), and very high (28.54%). In this context, it became important to better understand the activities performed by nursing technicians in the ICU.
The first step was to go to the gemba and use a Process Study Sheet to identify the variation in time spent performing each activity, the level of complexity, and whether the activity was routine or occasional—highlighting the experience and precision required to maintain safe, continuous care.
After identifying the processes and the time spent by each professional, an analysis of the “spaghetti flow” was conducted. It revealed a critical operational challenge in the ICU, especially during nursing technicians’ break periods. When one technician leaves for a break, the others must immediately assume responsibility for the patients assigned to that technician. This redistribution causes intense internal movement, directly impacting both work dynamics and care safety.
In practical terms, two critical moments were identified throughout the day. For a two-hour period, the ICU operated with only three technicians to care for 10 patients, which corresponded to 60% of the ideal operational capacity. This abrupt reduction increased the workload of the remaining professionals, who constantly had to move to ensure patient care, increasing the likelihood of delays and failures in the care process. During the same 8-hour shift, another, slightly less critical situation occurred during a one-hour period when the team had four technicians, reducing care capacity to 80%.
It is worth remembering that even in the previous scenario, with 6- and 12-hour shifts and five technicians and two nurses for every 10 ICU beds, staffing was still below what is ideal for an ICU, exposing the team to persistent risks and increasing pressure on professionals.
This complexity could be assessed using the NAS (Nursing Activities Score), which measures nursing workload. In 2022 and 2024, our NAS scores were 95% and 89%, respectively, corroborating the high level of complexity (between 80% and 100%).
The frequent movement of technicians to cover temporary absences directly impact efficiency and quality of care. Time spent moving, the need to quickly adapt to different demands, and physical and mental overload compromised our unit’s responsiveness. In addition, forced rotation risked breaking the continuity of care, impairing communication among professionals, and consequently compromising patient safety.
An analysis of the eight months prior (January to August 2022) and the seven months after (September 2022 to March 2023) the change in working hours provided a compelling scenario that reflected the impact of this change on operational indicators and employee perception.
The labor database, for example, showed a 600% increase in the issuance of medical leave certificates when comparing six-hour shifts with eight-hour shifts. According to Almeida & Rodrigues (2013), the average cost of absenteeism ranges from 2% to 6% of payroll. Projecting this to 2022, costs associated with medical leave increased from R$ 54,202.43 (US$9,600) to R$ 325,214.58 (US$58,000).
Another relevant finding showed a 380% increase in requests for transfer of ICU professionals to other sectors. Such high turnover affects team stability and generates a cascade effect: exhausting work leads to the search for transfers, resulting in the entry of inexperienced staff, which in turn further overloads more experienced professionals.
A third concerning point was a 450% increase in “near miss” notifications. In hospitals, this term—also called a “Near Adverse Event” or “Near Error”—refers to an incident that did not cause harm to the patient because it was detected and corrected before reaching them, signaling a process failure. This is a critical indicator, as it reflects a higher incidence of potential failures and implies a significant average cost per event. Based on a study by Zhan and other authors, a single adverse event can cost, on average, US$ 8,750. Projecting this to the 450% increase results in a substantial amount of US$ 39,375.
An analysis covering 2022 through one year after the change in working hours revealed alarming data: increases of 320% in the annual incidence density of Urinary Tract Infection (UTI), 54% in Primary Bloodstream Infection (PBSI), and 61% in Ventilator-Associated Pneumonia (VAP). This rise indicated that failures in the implementation and execution of prevention protocols were impacting multiple care fronts.
Clearly, the change in workload affected not only operational efficiency and safety but also the organizational climate. These results pointed to professional overload and deterioration of working conditions, which may compromise, in the long term, both quality of care and the financial sustainability of the ICU.
LEAN COUNTERMEASURES IMPLEMENTED
The first measure adopted was the development of an ideal state. For this, it was essential to map critical points at the gemba and build a consistent and realistic action plan covering different strategies.
The first countermeasure considered was the restructuring of shifts and hiring. The proposal provided for alternating 6-hour daytime shifts and 12-hour nighttime shifts, with the objective of reducing overload indicators. This plan included hiring new professionals: an estimated need for 15 technicians and 4 nurses to balance demand and improve quality of care.
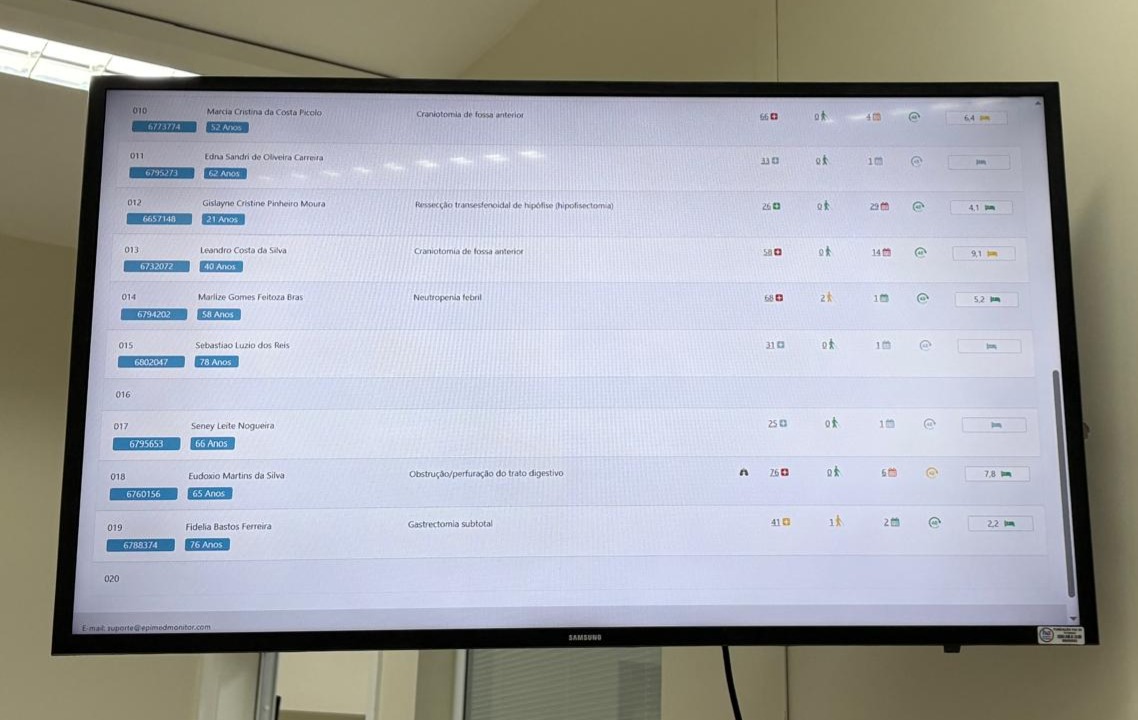
Visual management was also implemented, aiming to modernize manual processes such as recording vital signs and controlling medication entry and exit. The objective was to reduce workload and errors resulting from information loss. Visual management tools for monitoring inventories and flows—such as tracking length of stay and invasive devices—will enable fast and effective corrective actions.
Safety rounds or safety huddles were also introduced—quick, structured meetings held preferably at the beginning of the afternoon shift, where nurses, physiotherapists, physicians, and nutritionists meet to discuss the day’s critical points, review safety indicators, and anticipate potential risks.
Investing in regular training and holding daily meetings was also essential to raise awareness of good care practices and the prevention of adverse events. This approach seeks to create a continuous learning environment, increasing adherence to protocols and reducing error incidence, with a focus on patient care quality and professional safety.
One of the trainings developed was the formation of the Rapid Response Team for the ICU, a multidisciplinary team trained to recognize early signs of patient deterioration and take immediate measures for stabilization.
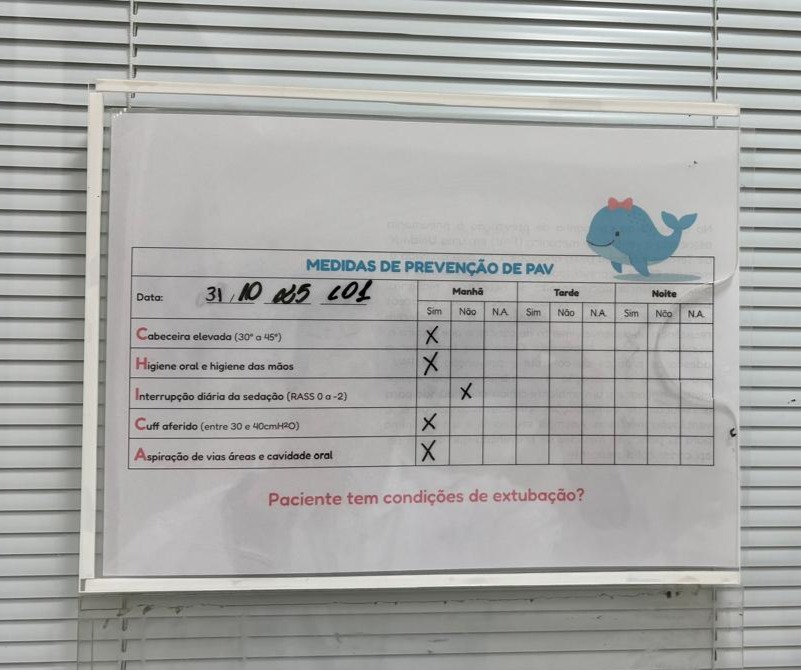
In response to the increase in HAIs, a project was implemented in January 2025 focused on training and raising awareness among the multidisciplinary team regarding Ventilator-Associated Pneumonia (VAP). The project involved active participation from nursing technicians, physicians, physiotherapists, nurses, dentists, and the Hospital Infection Control Service (SCIH), reinforcing an integrated approach to promoting patient safety. In the initial phase, the focus was on VAP awareness, highlighting risks and impacts on care quality. In the second phase, structured presentations were delivered to the entire team once per quarter in a meeting called Coffee without VAP, addressing evidence-based prevention strategies and promoting adherence to the VAP bundle.
The educational sessions were designed to train and develop open dialogue, stimulate reflection and professional commitment, and ensure effective implementation of preventive measures in daily hospital routines, keeping staff informed of indicator evolution.
It was also essential to promote monitoring of quality and satisfaction indicators and to closely follow results before and after interventions. Monthly meetings and quarterly reports enable identification of deviations and agile adjustments, ensuring continuous process evolution and transparency with the entire team.
THE RESULTS
HAI incidence density. The trend in VAP incidence density has been increasing in recent years, reaching a rate of 9.1 in 2024. However, the implementation of training focused on adherence to the VAP bundle and the expansion of awareness actions regarding HAIs promoted a significant change. After these interventions, the incidence rate dropped to 6.9, a reduction of 32.3%.
Medical leave and turnover. In 2023, Hospital de Amor recorded 168 certificates. In 2024, the number fell to 36.7—an improvement of approximately 78%. As for turnover, in 2023, after the shift change, 38 transfer requests were recorded, whereas in 2024, the annual rate averaged 31 requests. This reduction possibly reflects employee expectations regarding the proposal to return to the previous regime, as indicated by information collected from the team.
Standardized Mortality Ratio (SMR). To deepen analysis of care quality, an evaluation of the standardized mortality ratio was conducted, defined as the ratio between observed mortality and expected mortality according to SAPS 3. In 2024, this ratio was 1.11, indicating that observed mortality was 11% above the expected value. With the improvement initiatives implemented, the period from January to April 2025 recorded an SMR of 0.85, representing a reduction of about 23%.
The results achieved reflect significant advances in care practices and patient safety in the ICU. These gains demonstrate the importance and value of systematic and integrated continuous improvement approaches. By acting directly on waste elimination, strengthening teamwork, and maintaining a constant focus on quality and safety, Lean offers a structured path to transform critical challenges into opportunities for sustainable growth. This fosters a culture of operational excellence, respect for people, and, above all, safety for patients and professionals.
Read more


FEATURE – Looking to the future, the author encourages us to challenge obsolete ideas and seize the opportunity provided by Lean Thinking to make the world a better place for all.


FEATURE – In lean, we talk about PDCA all the time… but do we actually practice it as we should? The authors discuss what makes for successful continuous improvement.


FEATURE – Using an effective example from every-day life, the author discusses why Kanban is the gateway to Lean Thinking – and not just a tool.

GETTING TO KNOW US – It’s easy to over-complicate lean thinking. This month’s Lean Global Network interviewee tells us why we should always start with the work and the people doing it.
Read more


FEATURE – Thanks to Lean, EHA Clinics improved safety, efficiency, and patient experience. Now they’re hoping their results will inspire a growing movement to transform healthcare across Nigeria.


INTERVIEW – By making lean its way of thinking and acting, a hospital in Porto Alegre, Brazil was able to dramatically improve patient flow and transform its culture.


FEATURE – By using lean management, the Hospital São Francisco (HSF) near São Paulo, Brazil, has improved its ability to deal with dengue epidemics – treating patients more quickly and efficiently.


WEB SERIES – Today, we launch a new documentary series on lean around the world, with the first season focusing on lean in Brazil. In the first episode, we visit the lean clinic on a mission to reduce the burden on cancer in our lives.

